Gut-Brain Axis Studies: Understanding Its Role in Autoimmune Diseases and Immune Health
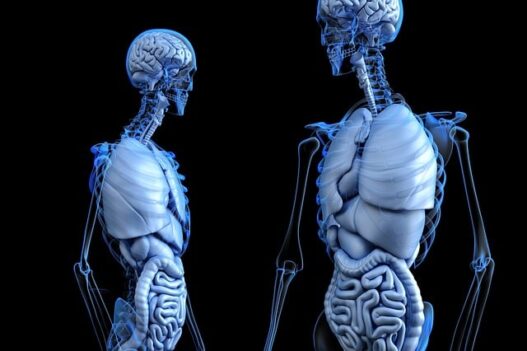
The Gut-Brain axis Studies explore to the bidirectional communication between the gut microbiota and the brain. It also studies how this relationship is influencing both neurological and immune functions. Disruptions in this axis can contribute to the pathogenesis of autoimmune diseases by altering immune responses and promoting inflammation. Emerging research suggests that restoring gut health through dietary changes and probiotics may have therapeutic potential for managing autoimmune conditions by enhancing immune regulation and reducing systemic inflammation.
The Gut-Brain Axis and the Microbiome: Mechanisms and Clinical Implications
Below is a study that analyzes the mechanism and clinical implications of the gut-brain axis on the microbiome.
Check out this fascinating video that explains the link between the gut microbiome and autoimmune diseases, offering valuable insights into this complex relationship.
The gut-brain axis connects the gut and brain, affecting both immune function and neurological health. Disruptions in this axis can trigger autoimmune diseases by altering immune responses and increasing inflammation. Recent research highlights how gut health influences autoimmune disease development, offering new therapeutic opportunities. The bidirectional communication between the gut and brain involves neural, hormonal, and immune pathways that affect inflammation. Studies show that a healthy microbiome supports immune regulation and may reduce systemic inflammation in autoimmune conditions.
Restoring gut balance through diet, probiotics, and lifestyle changes can help manage autoimmune diseases effectively. Emerging evidence suggests that gut health also influences mental health, including anxiety and depression in autoimmune patients. Probiotics, prebiotics, and anti-inflammatory foods may improve gut health and immune responses in autoimmune diseases. Research shows that early-life factors like diet and birth method affect gut microbiota development and immune function. Scientists are investigating how the gut-brain axis could lead to better treatments for autoimmune diseases.
Conclusion:
“Well-characterized bidirectional communication channels, involving neural, endocrine, and inflammatory mechanisms, exist between the gut and the brain. Communication through these channels may be modulated by variations in the permeability of the intestinal wall and the blood-brain barrier. Brain gut microbiome interactions are programmed during the first 3 years of life, including the prenatal period, but can be modulated by diet, medications, and stress throughout life. Based on correlational studies, alterations in these interactions have been implicated in the regulation of food intake, obesity, and in irritable bowel syndrome, even though causality remains to be established.
To further explore how the gut microbiome influences autoimmune diseases, check out our detailed blog on the role of gut microbiome studies.