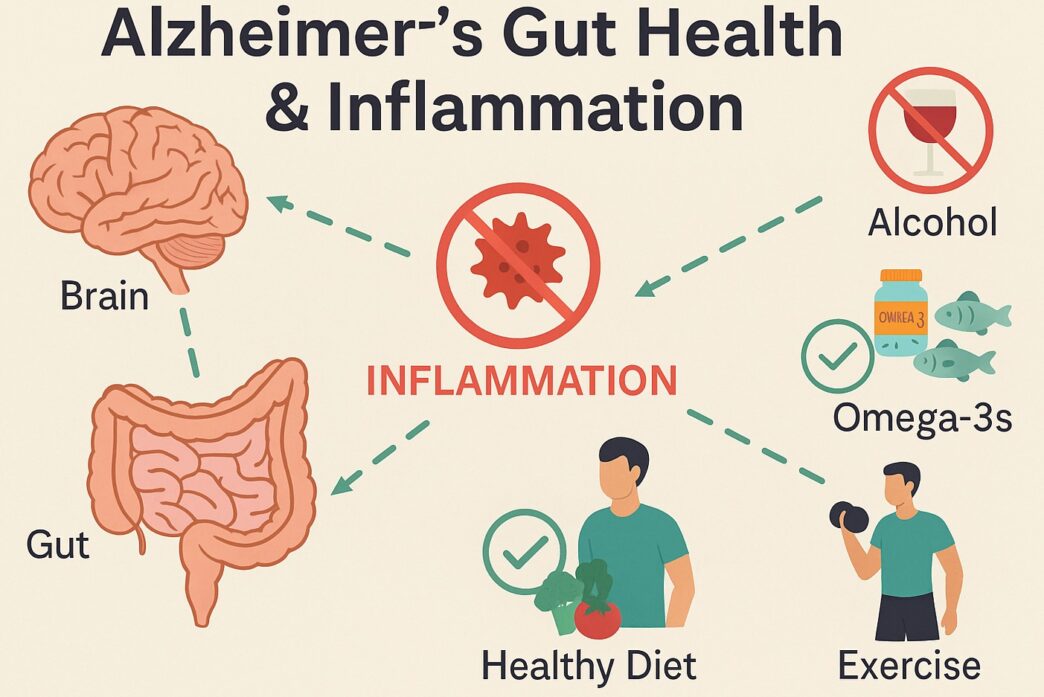
Alzheimer's Gut Health & Inflammation: What You’re Not Being Told
When someone close to you starts forgetting things they never would have forgotten before — a name, a birthday, how to get home — it does something to your heart. I’ve seen it happen. It’s a slow unraveling that makes you want to hold onto every memory just a little tighter.
Alzheimer’s is a disease that most of us fear — and with good reason. But what if we could do more than just fear it? What if we could take steps today that might lower our risk tomorrow?
That’s the question that sent me deep into the research on Alzheimer’s gut health & inflammation, and what I found completely changed the way I care for my brain… and my gut.
Early Signs of Alzheimer’s: Don’t Ignore These Clues
Before diving into the gut-brain connection, I want to share the early symptoms of Alzheimer’s that are often brushed off as “normal aging.” These signs are your body’s way of asking for help:
-
Forgetting newly learned information
-
Repeating questions or statements
-
Difficulty with problem-solving or planning
-
Trouble following familiar recipes or directions
-
Misplacing items and not retracing steps
-
Withdrawing from hobbies or conversations
-
Mood or personality changes (especially confusion, fear, or suspicion)
If you or someone you love is showing these signs, don’t panic — but don’t wait. Early intervention matters, especially when Alzheimer’s gut health & inflammation are part of the picture.

Alzheimer’s Gut Health & Inflammation and Autoimmunity: The Missing Link
One thing that’s rarely discussed — and close to my heart — is how autoimmune diseases may increase the risk of developing Alzheimer’s.
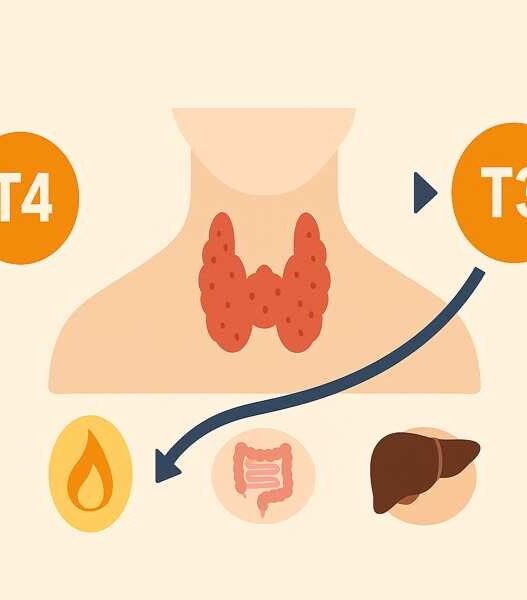
When you’re living with Hashimoto’s, autoimmune gastritis, or any chronic inflammatory condition, your body is already in a state of persistent immune activation. That inflammation doesn’t just affect the gut or thyroid — it can silently impact your nervous system and brain.
In a large study published in the Journal of Epidemiology & Community Health, researchers followed over 1.8 million people hospitalized with autoimmune diseases. They found that these individuals had a 20% increased risk of developing dementia later in life, especially vascular dementia, but also Alzheimer’s in some cases.
This research reinforces what I’ve seen personally and in the autoimmune community: if inflammation is left unchecked, it can move from the body into the brain. That’s why I believe managing autoimmunity isn’t just about symptom control — it’s about long-term brain protection. Alzheimer’s gut health & inflammation must be addressed early in people with autoimmune issues.
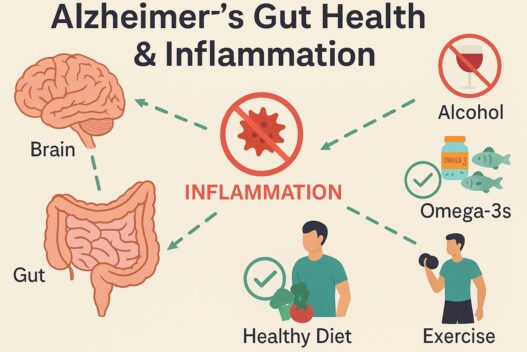
The Gut-Brain Connection in Alzheimer’s Gut Health & Inflammation
I used to think Alzheimer’s was all in the brain. But the more I learned, the more I realized: it may actually start in the gut. Your gut microbiome — the trillions of bacteria in your digestive tract — communicate constantly with your brain. And when that balance is disrupted, inflammation takes over.
Here’s what the science shows:
A 2018 study by Zhuang et al. found that Alzheimer’s patients had higher levels of harmful gut bacteria and reduced microbial diversity, especially in families like Firmicutes and Ruminococcaceae, which are known to reduce inflammation and protect gut integrity.
In a clinical trial by Akbari et al. (2016), 12 weeks of probiotic supplementation improved memory test scores in Alzheimer’s patients. Inflammatory markers also decreased.
A 2023 study by Fan et al. showed that individuals with mild cognitive impairment (MCI) had significantly fewer butyrate-producing bacteria, which play a role in regulating inflammation and protecting brain health.
These aren’t fringe studies. This is peer-reviewed research showing that gut dysfunction may contribute directly to Alzheimer’s risk — especially when paired with autoimmunity, blood sugar dysregulation, or chronic stress. Clearly, the gut is not just involved, it’s central to the conversation around Alzheimer’s Gut Health & Inflammation.
Alcohol’s Role in Alzheimer’s Gut Health & Inflammation
Let’s talk about alcohol — the one thing many people don’t want to give up, even when their body is asking for a break. I get it. I used to enjoy a glass of wine in the evening too. Now I drink alcohol only from time to time, when we meet with friends for special ocasions.
But once I started focusing on gut healing and brain clarity, I couldn’t ignore the research anymore:
- Alcohol promotes gut dysbiosis (more bad bacteria, fewer good ones)
- It damages the intestinal lining, increasing leaky gut
- It allows bacterial endotoxins (LPS) to reach the brain, where they trigger inflammation
- It contributes to neuroinflammation and brain aging, even at moderate levels
A 2023 narrative review published in the Journal of Gastroenterology and Hepatology confirms that alcohol disrupts the gut–brain axis, alters the gut microbiome, and plays a key role in neurodegeneration by increasing inflammatory signaling and oxidative stress.
This study also highlights how alcohol-induced microbial imbalance may be linked with neuropsychiatric symptoms and Alzheimer’s-related pathology through a dysfunctional vagus nerve-gut-brain pathway.
ARemoving alcohol gave me clearer thinking, better sleep, and much less brain fog. It was one of the simplest changes I made for Alzheimer’s gut health & inflammation prevention.
Brain-Protective Habits to Reduce Alzheimer’s Gut Health & Inflammation
I recently listened to a powerful interview on The Genius Life podcast with Louisa Nicola, a neurophysiologist who works with elite athletes and executives on cognitive performance. Her insights backed up what I’d already seen in my own healing, but she also taught me more.
Here are the key takeaways:
Strength Training Is Non-Negotiable
According to Louisa, resistance training is the most protective form of exercise for your brain. It builds muscle, which acts like an anti-inflammatory endocrine organ. It also increases BDNF (brain-derived neurotrophic factor) — essential for memory, learning, and neuroplasticity.
Too Much Cardio Can Backfire
While walking and light aerobic activity are great, she warned against overdoing high-intensity interval training (HIIT), especially if you’re inflamed or exhausted. Too much can raise cortisol and stress your brain.
DHA and EPA Are Essential
Omega-3 fatty acids — especially DHA — help build brain cell membranes. Louisa emphasized testing your omega-3 index and aiming for optimal levels through wild-caught fish or high-quality supplements.
Test, Don’t Guess
She recommended lab testing for insulin, homocysteine, CRP, omega-3 levels, and inflammatory markers. These tests help you spot red flags before symptoms show up.
Deep Sleep Is Brain Therapy
Lack of restorative sleep increases amyloid plaques in the brain. Louisa called sleep “the cheapest and most effective supplement we have for Alzheimer’s prevention.”
My Routine for Alzheimer’s Gut Health & Inflammation
If all this sounds overwhelming, let me make it simple. These are the things I’ve implemented in my own life and continue to follow today:
Cooked anti-inflammatory veggies daily: kale, cauliflower, cabbage
Bone broth and fermented foods (if tolerated) for gut support
Electrolytes and minerals to support energy and mood
Wild fish 3x/week
Strength training 3x/week
Breathwork and nervous system support every evening
Filtered water + sleep routine
No alcohol except special occasions, no processed sugar — my brain deserves better
Can Alzheimer’s Be Reversed? What the Research Says
Let’s be honest: full reversal is not possible once Alzheimer’s is advanced. But if you’re in the early stages — or even if you’re just noticing brain fog or forgetfulness — science shows it’s possible to slow, stabilize, or even slightly improve cognitive function.
The 2014 report titled “Reversal of Cognitive Decline: A Novel Therapeutic Program” describes a personalized protocol (now often referred to as the MEND program) that addressed metabolic and inflammatory factors underlying early-stage cognitive decline.
-
Among the 10 patients treated—many with mild cognitive impairment (MCI) or subjective memory decline—9 experienced subjective or objective improvements within 3–6 months.
-
Six who had difficulties or had to leave work were able to return to work or continue with improved performance. Improvements were sustained up to 2.5 years.
.This case series is one of the first to suggest that, particularly when caught early and treated comprehensively, cognitive decline may be slowed, stabilized, or even partially reversed. This proves that addressing Alzheimer’s gut health & inflammation early can lead to real, measurable improvements in memory and function.
We often wait for a diagnosis to change our lives. But what if we didn’t? What if we could start now — by caring for our gut, listening to our brain, and reducing the silent inflammation that fuels disease?
If you’ve felt that fear — the fear of forgetting, or watching someone you love slowly disappear — I want you to know: you’re not powerless.
Healing your gut, calming your immune system, and protecting your brain are all connected. And they’re all within your control.
Small daily actions matter more than we’ve been told.
If you liked this article you might also like to read: