Autoimmune Disease Risk Factors: Understanding Triggers and Taking Control of Your Health
Autoimmune Disease Risk Factors play a crucial role in understanding the triggers behind these conditions and how to manage them effectively. These Chronic Autoimmune diseases are complex and multifactorial, arising from a combination of genetic, environmental, and lifestyle factors. These diseases occur when the immune system mistakenly attacks the body’s own cells, leading to chronic inflammation and damage to various tissues and organs. Understanding the risk factors associated with autoimmune diseases can help in early detection, prevention, and management. In this article, we’ll explore the primary risk factors that contribute to the development of autoimmune conditions and discuss the roles of medication and diet in managing these diseases.
The Impact of Autoimmune Disease Risk Factors on Health and Wellness
Understanding these factors allows us to identify potential triggers and take proactive steps toward better health. Moreover, these risk factors often interact, amplifying their impact on immune function and overall well-being. Therefore, addressing risk factors like stress and diet can help minimize the likelihood of disease flares. In addition, lifestyle choices can either exacerbate or alleviate the impact of these risk factors on the immune system. By raising awareness, individuals can make informed decisions to support long-term health and disease management.
Autoimmune Disease Risk Factors:
1. Genetic Predisposition
Genetics play a crucial role in autoimmune diseases and is one of the Autoimmune Disease Risk Factors. Many individuals with autoimmune conditions have a family history of such diseases, suggesting a hereditary component. Specific genes are associated with an increased risk of autoimmune disorders. For instance, certain HLA (human leukocyte antigen) genes have been linked to conditions like rheumatoid arthritis, lupus, and multiple sclerosis.
Key Points:
- Having a family member with an autoimmune disease increases the risk.
- Certain gene variations can predispose individuals to specific autoimmune conditions.
Genetic Contribution:
- Research indicates that genetics may account for 10% to 30% of the risk for developing autoimmune diseases.
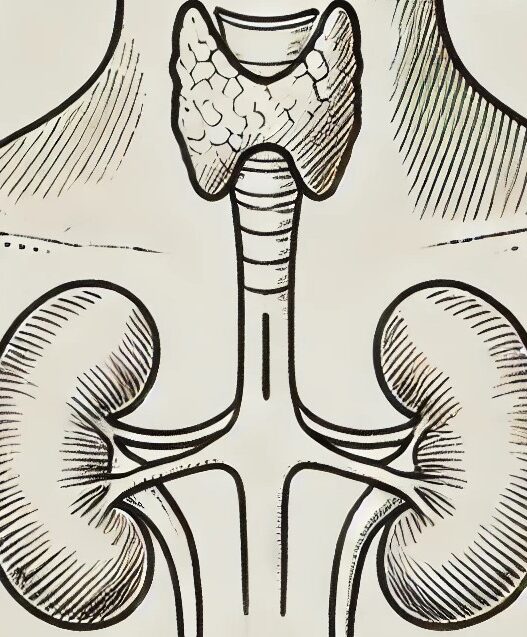
2. Gender
Gender is a significant risk factor, as autoimmune diseases disproportionately affect women. Approximately 75% of people with autoimmune disorders are female. Hormonal differences, particularly the influence of estrogen, are thought to contribute to this disparity. Conditions like lupus and Hashimoto’s thyroiditis are more common in women, especially during reproductive years.
Key Points:
- Women are at a higher risk for many autoimmune diseases.
- Hormonal fluctuations may play a role in disease onset.
3. Environmental Triggers
Environmental factors can trigger autoimmune diseases in genetically predisposed individuals. Environment plays an important role in the Autoimmune Disease Risk Factors. These triggers can vary widely and include:
- Infections: Certain viral and bacterial infections have been linked to the onset of autoimmune diseases. For example, the Epstein-Barr virus is associated with multiple sclerosis and lupus.
- Chemicals and Toxins: Exposure to environmental toxins, heavy metals, and certain chemicals (like pesticides and solvents) can increase the risk of autoimmune conditions.
- Diet: Some studies suggest that diets high in processed foods, sugar, and gluten may contribute to autoimmune disease development. Conversely, diets rich in anti-inflammatory foods (like fruits, vegetables, and omega-3 fatty acids) may help reduce the risk.
Key Points:
- Infections can trigger autoimmune responses.
- Environmental toxins and dietary factors play a role in disease development.
4. Stress
Chronic stress has been shown to impact immune function, potentially leading to the development or exacerbation of autoimmune diseases. Stress can trigger inflammatory responses and disrupt the balance of immune system function. Not taken seriously by the doctors, stress in one of the most important Autoimmune Disease Risk Factors. Events such as physical trauma, emotional distress, or prolonged stress can contribute to the onset of autoimmune conditions.
Key Points:
- Chronic stress can weaken the immune system.
- Stress management techniques, such as mindfulness, yoga, and therapy, may help reduce the risk of autoimmune flares.
5. Hormonal Factors
In addition to gender, hormonal changes during different life stages (such as pregnancy, menstruation, or menopause) can influence autoimmune disease risk. Some women experience flares of autoimmune conditions during hormonal changes, suggesting a connection between hormones and immune responses.
Key Points:
- Hormonal fluctuations can trigger or worsen autoimmune symptoms.
- Monitoring hormone levels and managing hormonal health may be beneficial.
6. Gut Health
The gut microbiome—the complex community of microorganisms in the digestive tract—plays a crucial role in immune function. An imbalance in gut bacteria (dysbiosis) can lead to increased intestinal permeability, often referred to as “leaky gut.” This condition allows harmful substances to enter the bloodstream, potentially triggering autoimmune responses. Factors such as diet, antibiotic use, and lifestyle can impact gut health.
Key Points:
- Gut health is linked to immune function.
- A balanced diet, rich in probiotics and fiber, may help support gut health and reduce autoimmune risk.
7. Vitamin Deficiencies
Certain vitamin deficiencies, particularly vitamin D and B12, have been associated with an increased risk of autoimmune diseases. Vitamin D is essential for immune regulation, and low levels are linked to conditions like multiple sclerosis and rheumatoid arthritis. Similarly, vitamin B12 deficiency can lead to autoimmune gastritis and neurological issues.
Key Points:
- Maintaining adequate vitamin levels is crucial for immune health.
- Regular screening and supplementation may be beneficial for at-risk individuals.
8. Age
The risk of developing autoimmune diseases can increase with age. Some conditions, like rheumatoid arthritis and lupus, are more commonly diagnosed in middle-aged individuals. However, autoimmune diseases can develop at any age, and some, like type 1 diabetes, are often diagnosed in childhood.
Key Points:
- Autoimmune diseases can occur at any age, but certain conditions are more common in specific age groups.
- Awareness of symptoms at different life stages can aid in early diagnosis.
9. Medication
The management of autoimmune diseases often involves medication to control symptoms and prevent disease progression. Commonly used medications include:
- Anti-inflammatory drugs: Nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce inflammation and relieve pain.
- Immunosuppressants: These drugs suppress the immune system’s activity to reduce tissue damage from autoimmune attacks.
- Biologics: Targeted therapies that focus on specific parts of the immune system, often used in diseases like rheumatoid arthritis and psoriasis.
While medication is crucial for managing autoimmune diseases, it’s important to work closely with healthcare providers to monitor for potential side effects and interactions. Personalized treatment plans can help ensure the best outcomes.
Key Points:
- Medications play a vital role in managing autoimmune diseases.
- Regular follow-up with healthcare providers is essential for optimal treatment.
10. Diet and Lifestyle
Diet and lifestyle choices significantly influence the risk and management of autoimmune diseases. A nutrient-dense, anti-inflammatory diet can help alleviate symptoms and improve overall health. Some dietary considerations include:
- Elimination diets: Identifying and eliminating food sensitivities (such as gluten, dairy, and processed sugars) can help reduce inflammation and symptoms.
- Anti-inflammatory foods: Incorporating foods rich in omega-3 fatty acids (like fatty fish, flaxseeds, and walnuts), antioxidants (like berries and leafy greens), and probiotics (like fermented foods) can support immune health.
- Hydration: Staying well-hydrated is essential for overall health and can help with symptom management.
- Exercise and sleep: Regular physical activity and adequate sleep are crucial for maintaining a healthy immune system and managing stress levels.
Key Points:
- A balanced diet can help reduce autoimmune symptoms.
- Lifestyle changes, including exercise and stress management, are vital for overall well-being.
Autoimmune Disease Risk Factors Conclusion
Autoimmune diseases arise from a complex interplay of genetic, environmental, and lifestyle factors. While genetic predisposition may account for approximately 10% to 30% of the risk for developing these conditions, lifestyle and environmental factors contribute significantly, accounting for around 70% to 90% of the risk. By understanding these risk factors, individuals can take proactive steps toward early detection, prevention, and management of autoimmune conditions.
While it may not be possible to eliminate all risk factors, adopting a healthy lifestyle—such as a balanced diet, regular exercise, stress management, and adequate vitamin intake—can help support immune function and reduce the likelihood of developing autoimmune diseases. Awareness and education are essential in navigating the challenges of autoimmune conditions, empowering individuals to seek appropriate care and live healthier lives. Through comprehensive approaches that include medication, dietary considerations, and lifestyle modifications, those affected by autoimmune diseases can better manage their conditions and improve their quality of life.
For a deeper understanding of how environmental factors contribute to the development of autoimmune diseases, the National Institute of Environmental Health Sciences (NIEHS) provides valuable insights. Their research highlights the role of environmental exposures—such as infections, toxins, and pollutants—in triggering autoimmune responses, particularly in those with a genetic predisposition. Exploring these environmental triggers can help identify potential prevention strategies and early intervention methods. To learn more, visit their detailed article on autoimmune disease triggers.
For more information you can also read my blogs:
Air quality and Autoimmune Health
Water Quality and Autoimmune Health
The Hidden Dangers of Mold Exposure